From the Gist Weekly team at Kaufman Hall
We hope that spring has sprung wherever you are! Publishing note: we’ll be away next week but will see you back here on Friday, April 5th. Please sign up to receive Gist Weekly directly in your inbox (nearly) each week.
In the News
What happened in healthcare recently—and what we think about it.
- Change Healthcare starting to bring systems back online after cyberattack. UnitedHealth Group (UHG) continues to restore the functionality of its Change Healthcare platform four weeks after a cyberattack led Change to shut down most of its operations. Change’s medical claims preparation software, electronic payments platform, and pharmacy network services have been relaunched to varying degrees, but more than a hundred services remained offline as of this past Monday. It’s expected to take months to restore all data from backup systems, identify and correct all damages caused by the hack, and process all backlogged payments owed to providers.
- The Gist: Over the past month, the impact of Change’s cyberattack on providers has become clear: 94 percent of hospitals report that the hack has financially hurt them, and nearly 60 percent report their level of financial impact to be at least $1M of revenue per day. As of this week, UHG has loaned more than $2B to providers in the form of advanced payments to ameliorate cash shortfalls. The Centers for Medicare and Medicaid Services (CMS) has also distributed nearly $3B in advanced Medicare payments, as lawmakers continue to pressure the Department of Health and Human Services to provide more help for affected providers. UHG now faces a federal probe into its cybersecurity and at least six class action lawsuits as a result of the cyberattack. The unprecedented scale of disruption caused by this hack will no doubt be a catalyst for healthcare cybersecurity reform.
- Elevance Health to buy Kroger’s specialty pharmacy business. On Monday, national supermarket giant Kroger announced that it had reached a definitive agreement to sell its specialty pharmacy business to insurer Elevance Health, which plans to fold the business into its CarelonRx pharmacy benefit manager (PBM) division. Kroger’s in-store retail pharmacies and walk-in clinics are not included in the deal, which could close in the second half of 2024. Kroger’s specialty pharmacy is the sixth largest by revenue, serving two percent of the US market. The planned sale comes as Kroger pursues a merger with rival supermarket chain Albertsons, which also operates a specialty pharmacy, although the Federal Trade Commission (FTC) recently announced that it’s challenging that merger.
- The Gist: With total pharmacy spend up 25 percent since 2019, including a 34 percent growth for specialty drugs, Elevance is capitalizing on a booming market by pushing into pharmacy services. Last year, the payer also acquired BioPlus, another specialty pharmacy. Administering high-cost drugs to patients with rare or complex diseases, specialty pharmacies now account for more than half of all prescription drug spending despite making up only around two percent of total prescription volumes.
- CMS launches new model to boost primary care ACOs. On Wednesday, CMS unveiled the ACO Primary Care Flex Model, which will offer participating accountable care organizations (ACOs)—whether new or renewing—in the Medicare Shared Savings Program (MSSP) a one-time, advanced payment along with monthly prospective payments, rather than shared savings at the end of a given performance year. Set to begin in January 2025, the five-year, voluntary model is targeted at “low-revenue” ACOs (as defined by their share of Medicare Parts A and B spending for assigned beneficiaries). The National Association of ACOs (NAACOS), which supports the ACO Primary Care Flex Model, has asked that CMS reconsider its exclusion of high-revenue ACOs, saying that the exclusion prevents independent primary care practices that have already joined a health system ACO from being able to access the benefits of the new model.
- The Gist: This new model is designed to better support smaller ACOs—which tend to be physician-only—by giving them access to a more stable cash flow. The highest-performing ACOs in the MSSP have been smaller, physician-only ACOs with relatively more primary care physicians and fewer specialists. With less than half of traditional Medicare beneficiaries in an ACO as of January 2024, CMS must entice more providers to join or form ACOs if it is to achieve its goal of getting every Medicare beneficiary into an accountable care arrangement by 2030.
Plus—what we’ve been reading.
- Health systems partnering with affordable housing developers. Published last week in the New York Times, this piece highlights a growing trend in health system community benefit provision: partnering with developers to build affordable housing. These partnerships have focused on a range of housing needs, from transitional housing for people experiencing homelessness, to housing for people who need special care, to affordable housing for hospital employees. Many of these projects also include co-located medical clinics to make it easier for residents to access healthcare services, and some are even being planned on health system-owned property.
- The Gist: Housing security has long been a significant social determinant of health, something that most providers recognize every day, given that a record number of Americans are currently experiencing homelessness. Among families with complex medical needs, stable housing was demonstrated to reduce adverse health outcomes in children by 20 percent. In addition to health systems, managed care organizations are also investing in different kinds of housing solutions, and at least 19 states are directing Medicaid dollars toward housing assistance.
Graphic of the Week
A key insight illustrated in infographic form.
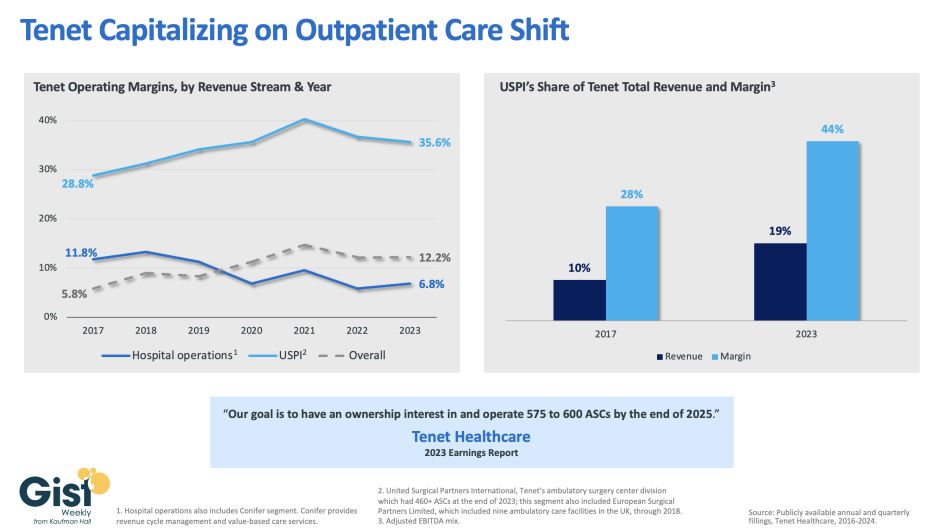
Tenet driving growth and profitability through ASC segment
In this week’s graphic, we dive into recently released data on Tenet Healthcare’s 2023 financial performance. While the for-profit healthcare services company’s annual margin on hospital operations has declined since 2017, its overall profitability has more than doubled, thanks to strong performances from its ambulatory surgery center (ASC) chain, United Surgical Partners International (USPI), which has consistently posted margins above 30 percent. Despite bringing in less than one fifth of Tenet’s total revenue, USPI is now responsible for almost half of Tenet’s overall margin. Tenet has pursued this growth aggressively since buying USPI in 2015, swelling its ASC footprint from 249 locations in 2015 to more than 460 in 2023, with plans to increase that number to nearly 600 by the end of next year. Tenet appears to be doubling down on its strategy of pursuing high-margin services over high-revenue services, especially as outpatient volumes are expected to far surpass growth in hospital-based care over the next decade.
On the Road
What we’re learning from our work in the real world. This week from Therese Fitzpatrick, Senior Vice President, at Kaufman Hall.
Incorporating more scheduling flexibility into bedside nursing
“This is not the same bedside nursing workforce I used to know,” a health system CNO admitted to me recently after a meeting. “COVID really changed things, especially for the crop of Gen Z nurses we’re hiring right now. They need more training, and they want more flexibility—which we’re trying to give them—but then they’ll probably leave us after just a few years.” Although the Gen Z job-hopping phenomenon exists across all industries, healthcare has been particularly challenged by post-pandemic labor disruptions as well as the new demands of our youngest generation of workers. “Thank goodness for our veteran nurses,” she went on to add, “but more and more of them are retiring, and I’m worried about filling our ranks.”
It's true that the nursing workforce has undergone massive changes in recent years, but I’m more optimistic about the future, even if it comes with some near-term growing pains. There’s definitely a rising group of nurses, often younger and less experienced, who want maximum flexibility from their job. This can include atypical shift lengths and start times, opportunities to travel for more pay, and often an expectation that a job is just one of many stepping stones in a long career. But there is also still a group of nurses who value predictability and stability, preferring to work in the same unit for the same shifts each week. The trick for hospitals trying to please both of these groups is to offer flexibility flexibly: build staffing plans around a core group of workers, which will likely come to include more Gen Z employees as they age, and then supplement with varied shift options to shore up staffing levels wherever needed. In theory, these dual scheduling tracks should increase labor efficiency, although in practice, designing these schedules gets very complicated, very quickly. If you’re looking to implement more flexible scheduling for bedside nurses, don’t hesitate to reach out.
On our Podcast
Gist Healthcare Daily—All the headlines in healthcare policy, business, and more, in ten minutes or less every weekday morning.
Last Monday, host J. Carlisle Larsen spoke with Zachary Fleitman, founder and CEO of talent pipeline management platform WorkUp Health, which provides health systems with a customizable app to help them track and evaluate the impact of their student outreach initiatives.
This coming Monday and Tuesday, we revisit JC’s two-part conversation from last fall with Sara Vaezy, Executive Vice President and Chief Strategy and Digital Officer for Providence. They discuss the Providence Digital Innovation Group’s latest incubated company—Praia Health—a platform-as-a-service technology that aims to increase patient engagement.
And be sure to tune in every weekday morning to stay abreast of the day’s biggest healthcare news. Subscribe on Apple, Spotify, Google, or wherever fine podcasts are available.
Thanks for tuning in to another week of news and analysis! We’ll be back with a new Gist Weekly edition the first Friday in April.
Best regards,
The Gist Weekly team at Kaufman Hall






